Vesicovaginal Fistula
Vesicovaginal Fistula
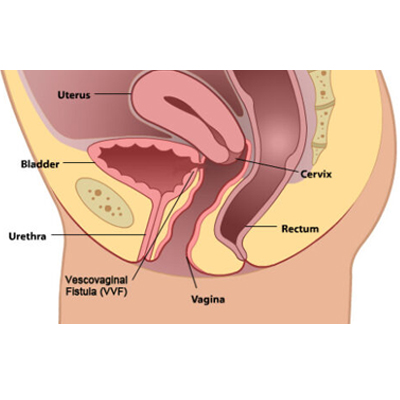
A vesicovaginal fistula (VVF) is an abnormal connection or passageway between the urinary bladder and the vagina. It typically occurs as a result of injury or trauma to the tissues that separate these two structures, leading to the formation of a hole or communication between them. This abnormal connection allows urine to pass from the bladder into the vagina, resulting in urinary incontinence.
Vesicovaginal fistulas can be caused by various factors, including:
1. Obstetric injury: Prolonged or difficult labor, particularly when accompanied by prolonged pressure of the fetal head against the maternal pelvis, can lead to tissue damage and the formation of a fistula.
2. Gynecological surgery: Complications from certain gynecological procedures, such as hysterectomy, may result in vesicovaginal fistulas.
3. Radiation therapy: Pelvic radiation therapy for the treatment of gynecological or colorectal cancers can cause damage to the tissues, leading to the formation of a fistula.
The main symptom of a vesicovaginal fistula is continuous urinary leakage through the vagina, which can result in significant social, psychological, and physical distress for affected individuals. Other symptoms may include recurrent urinary tract infections, irritation or inflammation of the vaginal tissues, and an ammonia-like odor.
The treatment for vesicovaginal fistula typically involves surgical repair. The specific approach depends on factors such as the size and location of the fistula. In some cases, minimally invasive techniques may be used, while larger or more complex fistulas may require open surgery. The goal of the surgery is to close the fistula and restore normal urinary function.
After the repair, it is important to monitor the patient for complications such as infection or recurrence of the fistula. In some cases, additional procedures or interventions may be needed to achieve a successful outcome.
It's worth noting that while vesicovaginal fistulas can have a significant impact on a person's quality of life, they are generally treatable. Seeking medical attention from a qualified healthcare professional, such as a urologist or gynecologist, is crucial for diagnosis and appropriate management of vesicovaginal fistulas.